
The Hidden Public Health Problem of Inadequate Sleep: Deploying Digital Mobile Technology to Improve Employee Sleep Hygiene in Asia
*Corresponding Author(s):
George A GellertWellteq, Australia, Canada, Singapore, United States
Tel:+1 210 382 1664,
Email:ggellert33@gmail.com
Abstract
Objective
To evaluate the impact of an on demand, digital mobile application deployed via smartphone on the sleep hygiene and nightly duration of employee program participants within a large multinational banking enterprise.
Methods
A sleep duration improvement program was implemented using a smartphone application with the employee population of one of the largest digital banks in Asia, and across 13 nations of East, South and Southeast Asia. Participating employees were challenged to record and improve their sleep duration competitively over a 7-day period. The intervention method employed to encourage employees to engage included providing easy to assimilate, timely education on the criticality of sleep health, and conveying and reinforcing supportive motivational messaging at critical junctures. Straightforward messages imparted specific, personalized and practical educational content, tips, and resources around the importance and “how to” of improving sleep habits/hygiene and reducing disrupted and disordered sleep. Personal performance statistics were conveyed to each employee user, and awards and incentives deployed to increase program compliance and completion. Participants’ sleep duration was primarily recorded objectively via wearables (i.e., Garmin, Fitbit, and Apple smartwatches or fitness trackers), or subjectively through self-reporting within the mobile application.
Results
There were 529 employee participants who engaged the sleep week challenge in 13 nations and 8 enterprise markets across the Asian-Oceanic region. All markets within all nations showed a nightly sleep duration improvement. Fifty-nine percent (312) of all employee participants improved their average nightly sleep duration. The weighted average sleep duration increase was 38 minutes of nightly additional sleep achieved. Based on an initial average sleep duration of 7 hours, this represents a 9% increase in weighted average nightly sleep duration. Among the 232 (or 44%) of all employee participants who completed the entirety of the sleep week challenge, 71% recorded an increase in weighted average sleep duration versus their baseline sleep times.
Conclusion
The digital mobile employee engagement and program implementation evaluated in this study delivered a clinically meaningful improvement in employee sleep duration, and thus overall sleep health and wellness. Because of the automation and rules-driven customization enabled by web-based digital media, programs to improve population sleep hygiene can be deployed rapidly at scale across large employee/enterprise populations in multinational settings. These results and impact achieved after a single 7-day sleep challenge across a complex multinational and multicultural employee and enterprise setting are indicative of the power and value that digital mobile wellness engagement can deliver to employees.
Keywords
Employee wellness; Remote patient monitoring; Sleep health and hygiene
Introduction
The Critical Importance of Employee Sleep Duration, Quality and Hygiene
Sleep is a fundamental physiological and restorative process that affects many areas of health and cognition. Poor sleep hygiene and insufficient sleep each night can affect general health, immunological defenses, cardiovascular health, metabolic health, mental health and ability to cope with stress and depression, risk of cancer, experience of chronic pain, overall mortality, and human operational performance [1-3]. Sleep hygiene refers to a set of behavioral and environmental recommendations that are intended to promote healthy sleep [1-6]. For example, avoiding stimulants like caffeine and putting away screens before bed, which disrupt circadian rhythms, promotes good sleep hygiene [2, 4].
Decades of evidence demonstrate that individuals who have a nightly sleep duration of 7-8 hours are at lower overall mortality risk relative to individuals sleeping less than seven hours (or more than eight hours) [7]. Lack of sleep has been associated with a range of risks affecting employee wellness and job performance, including industrial and civil disasters, motor vehicle crashes, psychological distress, psychiatric conditions, drug and alcohol abuse, overall excess mortality and morbidity, increased avoidable health care utilization and costs, a reduction in overall wellness and wellbeing, decreased productivity and direct economic costs to the enterprise [1,7-9] In addition, getting an adequate amount of sleep is associated with increased cognitive and memory function [10].
Employees in occupational positions with higher job demands and low perceived job control are associated with having lower sleep quality [11]. Evidence suggests that, especially among employees in jobs requiring they work outside normal operational hours (i.e., working in the early morning, evening, and night), there may be a particularly elevated risk for occupational accidents and injuries, poor job performance, weight gain, type 2 diabetes, and heart disease due to chronic lack of sleep and disruptions of natural–and essential–circadian rhythms [12]. Employee problems with sleep can be a major contributor, along with unhealthy lifestyle choices, to increased avoidable employer costs due to short-term sickness-related absences by 10-30% [13].
Thus, assessing and improving sleep hygiene and duration are central objectives for Wellteq when implementing employee wellness solutions and challenges for clients. One method Wellteq utilizes for improving employee sleep hygiene involves a challenge program called Sleep Week, where participants log their nightly sleep duration for at least five out of seven days in a week, or this data is captured and reported automatically by a wearable device that accurately monitors sleep duration.
Methods
Effectively Converging Engagement, Education, Incentives and Technology to Improve Sleep Duration and Hygiene
Intervention Objectives and Technology Deployed
An on demand, digital interactive mobile application was deployed via smartphone to engage, educate, socially connect and motivate employees in a sleep health and hygiene improvement program. The application and platform used to deliver the intervention suite and to capture impact data was a white label of the Wellteq smartphone application. Willis Towers Watson provided consultancy across the deployment of the program with a particular focus on client insights. The program objective was to drive specific improvements in nightly sleep duration and quality (as manifest by sleep continuity), and then measure the impact of the digital sleep health/hygiene promotion program. The most frequently used vehicle engaged by participants to receive communications and share their data was their personal smartphones. The Figure 1 below shows several of the primary and most frequently used functionalities through which participating employees were engaged for conveying education and motivation to drive sleep behavior change.
 Figure 1: Mobility of Engagement, Content Delivery, Functionality, and Impact Measurement.
Figure 1: Mobility of Engagement, Content Delivery, Functionality, and Impact Measurement.
Study Setting
The sleep improvement program, or employee “Sleep Week Challenge”, was implemented within the employee population of one of the largest banks in East, South and Southeast Asia, and one of the mostly highly regarded digital banks in the world.
Study Participants and Selection
There were 529 employee participants who engaged the Sleep Week Challenge in 13 nations and 8 enterprise markets across the Asian-Oceanic region. The countries/markets where participants were located include Australia, China, Hong Kong, India, Indonesia, Japan, Malaysia, Singapore, South Korea, Taiwan, Thailand, U.S.A., and Vietnam.
Intervention Content and Outcomes Metrics Captured
The Sleep Week challenge was designed based on peer reviewed scientific evidence of behavioural responsiveness and sustained behavioural uptake and included various metrics including attitudinal/perception and knowledge-based indices, and wearable device physiological measurements of sleep duration indicators. Participating employees were challenged to record and improve their sleep duration over a 7-day period. Personal performance statistics were conveyed to each employee user, and awards and incentives deployed to increase program compliance and completion. Those able to achieve an average of 7 hours or more over 5 days had a chance to win prizes such as gift cards and similar financial incentives. Participants’ sleep duration was primarily recorded objectively via wearables (i.e., Garmin, Fitbit, and Apple smartwatches or fitness trackers), or subjectively through self-reporting within the mobile application.
The intervention method employed to encourage employees to engage and participate over the course of the Sleep Week challenge included providing easy to assimilate, timely education on the criticality of sleep health, as well as conveying reinforcing and supportive motivational messaging at critical junctures. Straightforward messages imparted specific, personalized practical educational content, tips, and resources around the importance and “how to” of improving sleep habits/hygiene and reducing disrupted and disordered sleep.
These resources were conveyed to participants via email and in-application notifications within the mobile application. Selected notifications were delivered as a push-notification, keeping the sleep challenge front of mind and supporting behaviour change with reminders, accountability, and support. Research shows that using push notifications is highly effective in encouraging user engagement in mental health and wellbeing apps [14]. The sleep challenge thus combined support and motivation via push notifications with sleep metrics reporting and group psychosocial support.
Different types and frequency of program outreach, and frequency of outcomes data capture, can be defined and implemented within the mobile application and platform according to enterprise objectives in a highly customized and individualized manner, as illustrated in Figure 2 below. Individuals are able to track their sleep through their dashboard which shows the metric of hours slept each night. Running the program across the company provided group psychosocial support. Knowing that all application users could be engaged in the same wellness or sleep challenge creates a safer environment and more social support to participate.
Figure 2: Program Samples of User Sleep Engagement, Education and Monitoring.
Results
Demonstrated Improvement in Average Sleep Duration in a Multinational, Multiregional Financial Services Industry Leader
All eight markets across all 13 participating nations showed sleep improvement, with an average duration of 7 hours of sleep across the week-long program, as shown in the Figure 3 (DAH2 and DBIL are regional markets in India; International Centres include the markets of Australia, Japan, Malaysia, South Korea, Thailand, U.S.A. and Vietnam).
In Figure 3, all time baseline refers to each participant’s average sleep duration since they joined the platform between January and August of 2021. Synching sleep data was not required before the challenge, but encouraged, therefore each participant had a different amount of data to average. This metric was largely impacted by whether a participant used a Garmin, Fitbit or other device connected to Apple Health. Others manually recorded their hours slept through the in app mind rating.
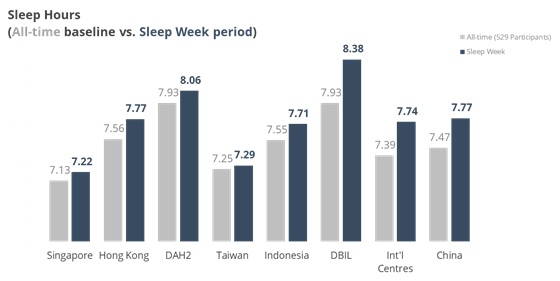 Figure 3: Sleep improvement among all employee challenge participants.
Figure 3: Sleep improvement among all employee challenge participants.
Fifty-nine percent (312) of all employee participants improved their average nightly sleep duration. The weighted average sleep duration increase was 38 minutes of nightly additional sleep achieved. Based on an initial average sleep duration of 7 hours, this represents a 9% increase in weighted average nightly sleep duration, as shown in Table 1.
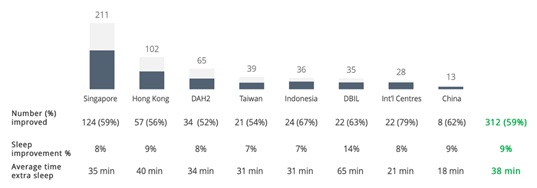 Table 1: Level of sleep duration increase among employees with improved sleep.
Table 1: Level of sleep duration increase among employees with improved sleep.
As seen in Table 2, among the 232 (or 44%) of all employee participants who completed the entirety of the Sleep Week challenge, 71% recorded an increase in weighted average sleep duration versus their baseline sleep times.
 Table 2: Sleep duration increase among employees completing the 7-Day sleep challenge.
Table 2: Sleep duration increase among employees completing the 7-Day sleep challenge.
Discussion
Employee Health Improvement and Risk Reduction Requires a Discrete Focus on Sleep Hygiene
The digital mobile employee engagement and program implementation evaluated in this study delivered a clinically meaningful improvement in employee sleep duration, and thus overall sleep health and wellness. Because of the automation and rules-driven customization enabled by web-based digital media, programs to improve population sleep hygiene can be deployed rapidly at scale across large employee/enterprise populations in multinational settings to achieve employee health and wellness objectives. Research evidence supports the expectation that improving sleep duration and hygiene may favorably influence employee safety, satisfaction, productivity and performance [1,7-9,11-13,15,16].
These results and program impact achieved after a single 7-day sleep challenge across a complex multinational and multicultural employee and enterprise setting are indicative of the power and value that digital mobile wellness engagement can deliver to employees. The findings illustrate how high value programs deploying this technology can impact across general physical and mental health wellness, targeted health promotion focused on chronic disease prevention and specific risk reduction, occupational injury and the associated avoidable health care utilization and enterprise costs [1,7-9,11-13,15-19].
Enterprise and employer Net Promoter Scores (NPS) can be captured during the implementation of diverse wellness and risk reduction programs for employees. An enterprise’s NPS is the likelihood of an employee recommending the employer or organization to others [20]. This increase in positive, beneficial employee perceptions of the enterprise and their employer can contribute meaningfully to improved employee job satisfaction and retention, while reducing avoidable costs due to employee turnover [21].
Conclusion
The Future of Sleep Medicine and Employee Health is here, and it is Digital
This case study quantitatively and compellingly demonstrates the impact, utility and value of digital mobility deployed against a difficult to modify behavior in non-clinical settings, including at home and the workplace for improvement of poor sleep habits, hygiene and inadequate duration. Given that insomnia, disrupted sleep and clinical sleep disorders are significant predictors of workplace accidents, and are contributors to acute and chronic mental health conditions such as stress, anxiety, and depressive disorders, the increase in average sleep duration achieved within the participating employee cohort was clinically meaningful [15].
The digital mobile employee engagement strategy used in this sleep health and hygiene improvement program aligns well with emerging digital remote monitoring technological capabilities to evaluate clinical sleep disorders, such as Obstructive Sleep Apnea (OSA), within the natural environment of the individual’s home. For sleep disorders, digital mobility and remote monitoring using unobtrusive wearable devices offer a less artificial setting for clinical sleep assessment versus a physician’s office-based sleep laboratory using highly intrusive Polysomnography (PSG). The use of remote monitoring technology also establishes a highly cost-effective ability to extend clinical observation of sleep quality and disruption from the single night data capture of the sleep clinic using PNG to recurrent, ongoing sleep quality evaluation in the home.
Driving this new capability to measure the quality and duration of sleep has been the emergence of a variety of wear able devices with internet connectivity to share data captured. Technology innovation and wearable advancement in recent years have involved remote patient sleep quality/duration monitoring, and OSA assessment using oximetry, monitoring of body movements during sleep (actigraphy), chest motion/respiratory monitoring, heart rate monitoring, Electroencephalography (EEG), Electromyography (EMG) and measurement of Peripheral Arterial Tone (PAT). In the coming years it is entirely possible that a combination of these remote monitoring technologies may displace the current gold standard of a patient having to spend one or more nights in the uncomfortable and artificial environment of a clinical sleep laboratory using PSG.
In 2022, the technology platform used in this employee sleep improvement program will evolve its multimodal wearable and data integration hub to expand the range and kind of physiological data streams captured, and will include an unprecedented suite of biometric parameters and measures indicative of sleep health and disruption.
Acknowledgement
The authors are grateful to the enterprise leaders and employees who participated in this digital sleep duration and quality improvement program.
References
- Grandner MA (2017) Sleep, health, and society. Sleep Med Clinic 12: 1-22.
- Morgenthaler T, Kramer M, Alessi C, Friedman L, Boehlecke B, et al. (2006) Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine Report Sleep 29:1415-1419.
- Banks S, Dinges DF (2007) Behavioral and physiological consequences of sleep restriction. Journal of Clinical Sleep Medicine 3:519-528.
- Stepanski EJ, Wyatt JK (2003) Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev 7: 215-225.
- Jefferson CD, Drake CL, Scofield HM, Myers E, McClure T, et al (2005) Sleep hygiene practices in a population-based sample of insomniacs. Sleep 28: 611-625.
- Gellis LA, Lichstein KL (2009) Sleep hygiene practices of good and poor sleepers in the United States: an internet-based study. Behav Ther 40:1-9.
- Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH (2015) The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med Review 22:23-36.
- Grandner MA, Hale L, Moore M, Patel NP (2010) Mortality associated with short sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med Review14: 191-203.
- Magnavita N, Garbarino S (2017) Sleep, health and wellness at work: A scoping review. Int J Environ Res Public Health 14: 1347.
- Walker MP (2009) The role of sleep in cognition and emotion. New York Academy of Science 1156:1681-197.
- Van Laethem M, Beckers DG, Kompier MA, Dijksterhuis A, Geurts SA (2013) Psychosocial work characteristics and sleep quality: A systematic review of longitudinal and intervention research. Scandinavian Journal of Work, Environment & Health 39: 535-549.
- Kecklund G, Axelsson J (2016) Health consequences of shift work and insufficient sleep. British Medical Journal 355.
- Kanerva N, Pietiläinen O, Lallukka T, Rahkonen O, Lahti J (2018) Unhealthy lifestyle and sleep problems as risk factors for increased direct employers’ cost of short-term sickness absence. Scandinavian Journal of Work, Environment & Health 44: 192-201.
- Auf H, Dagman J, Renström S, Chaplin J (2021) Gamification and nudging techniques for improving engagement in mental health and well-being apps. International Conference on Engineering Design 1647-1656.
- Garbarino S, Tripepi G, Magnavita N (2020) Sleep health promotion in the workplace. Int J Environ Res Public Health 17: 7952.
- Redeker NS, Caruso CC, Hashmi SD, Mullington JM, Grandner M, et al. (2019) Workplace interventions to promote sleep health and an alert, healthy workforce. J Clin Sleep Med 15: 649-657.
- Kakinuma M, Takahashi M, Kato N, Aratake Y, Watanabe M, et al. (2010) Effect of brief sleep hygiene education for workers of an information technology company. Ind Health 48:758-765.
- Capezuti EA (2016) The power and importance of sleep. Geriatric Nursing 37: 487-488.
- Hosker DK, Elkins RM, Potter MP (2019) Promoting Mental Health and Wellness in Youth Through Physical Activity, Nutrition, and Sleep. Child Adolesc Psychiatr Clin N Am 28: 171-193.
- Reichheld FF (2003) The one number you need to grow. Harvard Business Review.
- Gupta S, Zeithaml V (2006) Customer metrics and their impact on financial performance. Marketing Science. 718-739.
Citation: Gellert GA, Montgomery S, Gillett J, Gellert TE, Hole J, et al. (2021) The Hidden Public Health Problem of Inadequate Sleep: Deploying Digital Mobile Technology to Improve Employee Sleep Hygiene in Asia. J Community Med Public Health Care 8: 098
Copyright: © 2021 George A Gellert, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

